Chapters and Real Time Transcription
You are in week one of the four week bariatric education module.
I am Veronica Kasinek.
I am the registered dietitian at the OB City Medicine and Diabetes Institute.
And my area of involvement is bariatric surgery.
So that's why we are hanging out today.
And for the next four weeks, we're. Going to have Dr.
Galindo, one of our internal medicine doctors,
be our clinician, also with our groups for the next four weeks, which is amazing.
So I'm in the middle.
That's me.
To my left is Philip.
And Philip is really kind of our admin clinical case manager.
So he and Linda, I should add Linda's photo now
managethbariatricanmedweight CA so if you have any questions, if you're confused,
if you're lost, if you're not sure if bariatric surgery is for you,
just message them and they'll be able to guide you in regards to any questions
you have with our bariatric surgery stream.
And then on my right there, I have Dr.
Galindo, who will be with us answering any
medical related questions associated with bariatric surgery.
So this module is really kind of a bit
of an overview to help you really decide, give you the information.
And then following this four week module,
we have the bariatric preparedness course, which, where we work with our patients.
And at the end of that eight weeks,
hopefully, they'll be nuclear for the nutrition and lifestyle
and be referred to the Richmond Metabolic and Bariatric Surgery program.
So, again, kind of the goal is we want
to optimize your surgical outcomes and equip you to handle kind
of the challenges of your new life following bariatric surgery.
I'm probably going to give you details not in week three, but next week.
Philip is away right now, so I need to speak to him.
And so any questions?
I'm not going to answer about
the bariatric preparedness course till next week.
The outline for today is we're going
to really briefly review the bariatric surgery procedures.
Kind of. What are the.
There's actually four different types of bariatric surgery procedures
that the RichmonD metabolic and bariatric surgery program does.
We're also going to talk about kind
of the qualifications and pathway to bariatric surgery.
We're going to review the nutrition and eating behaviors that are required
and set forth for referral by the Richmond Metabolic and Bariatric Surgery program.
And these requirements.
Patients have heard that we have an expedited program.
And really, what that means is you're
in our program and you're already working towards bariatric surgery.
If you hadn't gone through your program
and you were waiting for a referral from your physician,
it's about a two and a half, three year wait to get to Richmond.
So you're already working on that path,
being in the bariatric stream in our program.
And so then when you get to.
To, you're still going to meet with their team, but it will be.
Yeah, fewer visits than if you were coming directly from a GP referral.
What are some of your first thoughts about bariatric surgery?
Or what have you heard about it before?
So what are some things that come up when we say bariatric surgery?
So, in our program, and if you start looking
at the Canadian Medical association, the World Health Organization,
the American Medical association, we all see kind of obesity as a chronic disease.
And the reason for that is that physicians
and doctors are really good at managing chronic disease, right,
where they are now starting to become more engaged and understanding it.
And even Obesity Canada came out in 2020.
In August 2020,
you can go to their website, and they've even developed the new adult
clinical practice, obesity guidelines for physicians and GPs
to help better, help take care of our patients.
So it's actually not no longer a pyramid, and I wasn't able to get the new graph,
but there are kind of three different ways that we manage obesity.
Right. So there's the bottom part,
or kind of the foundation, as we like to say, kind of the behavioral.
So eating, physical activity,
mental health, stress management, and sleep hygiene.
But we know that that alone only gives us a certain percent of weight loss.
And again, because of certain
physiological changes that happen in the body, weight often comes back.
Right. So weight loss and weight maintenance,
believe it or not, are two different physiological processes.
If you want to learn more about obesity medicine and the condition,
I welcome you to it, because fat doesn't just sit there.
It's an endocrine organ, and it also depends on what type of fat
you have and where it's located, where we then can impact our health conditions.
So then we have pharmacotherapy and we're seeing up to 20% weight loss,
and we have a lot of patients on different medications.
So we add that in also.
And then on top of that,
we have bariatric surgery, where we often see the most substantial
weight loss and definitely a tool to help keep that weight off and significant
improvements in kind of other health related conditions.
So I'm just going to review the digestive
process, because it's really important when we talk about the surgery and
the digestive system, how we're going to change it.
So going back to biology class or
nutrition one on one, we're going to talk about
how we have a normal digestion and then how we alter it.
So food goes into the mouth, where it is digested,
where we actually have amylase enzymes, and starch is already starting to be
digested in your mouth, and that begins to occur.
So if you've ever had a cracker and you
let it kind of sit and chew it for a really long time,
it might start tasting a little sweet, because we have the amylase enzymes
that are already starting to break down the starch following.
After that, we swallow food,
and it passes through the pharynx and travels down the esophagus,
where we have a sphincter, and then it lands in the stomach.
So in the stomach has several functions.
It's kind of the holding compartment for the food.
Food is already, again further digested partially through the churning action.
There are protease enzymes, pepsin, which start to break down protein.
And then after that, we have what we call gastric emptying as
food passes through the pyloric sphincter into the small intestine.
So in the small intestine, there's three parts to it.
The first part is the duodenum.
Then we have the diginum and the ilium.
And the most important role of the small intestine is vitamin and mineral
absorption, and also in the colon, water reabsorption.
So with bariatric surgery, when we talk.
About the surgeries, if we are impacting
the small intestine, where food is going to bypass part
of the small intestine, this is where you may have heard
that we're going to have a certain amount of nutrient malabsorption.
And then our undigested food passes
on to the large intestine, where water and electrolytes are absorbed
and our feces begin to form stools or poop.
And then the rectum holds the feces and the anus expels the stored feces.
Then we have the liver, which makes bile.
We also have a gallbladder that stores and concentrates the bile.
And some people have had their gallbladders removed.
And then we also have the pancreas, which makes enzymes for the small intestine.
So when it comes to bariatric surgery, we need to think about that.
We're kind of changing a bit the physiology of the digestive system.
And so bariatric surgery can help overcome the physiological changes that we see
with weight loss and produce significant and durable weight loss.
We also see significant improvements or resolutions in obesity related
comorbidities and also changes in life expectancy.
So the literature has shown about seven.
Years in women and five and a.
Half years in men.
And bariatric surgery kind of defeats
the powerful mechanisms we have for the defense against starvation
that can be inappropriately overactive in obesity.
So, for example,
we have different appetite hormones that may kick into high gear once we lose
weight, that may heighten the smell of food, taste of food,
want of food, which may make it harder to maintain weight loss.
Yes. Seven years added for one.
So the three surgeries
that are done at the Richmond Metabolic and bariatric Surgery program is
the sleeve gastrectomy, the root tone y gastric bypass,
and the biliopancreatic diversion and duodenal switch.
There's actually a new kid on the block,
a new surgery, which I'll mention in a moment,
and I'm not sure if doctor at the medical and surgical group,
if they talk about the saddi yet, but I will mention it today.
So, the sleeve gastrectomy is a procedure that they're all done laparoscopically.
So kind of a keyhole technique under a general anesthetic.
They make small,
five small incisions where they kind of insert keyhole surgery instruments.
And during this surgery,
they remove about 75% to 80% of your stomach, or the fungus of the stomach.
And so your new stomach sleeve,
which is similar to this shape of a tube or banana, holds about 125 beginning.
So about a half a cup of food.
The sleeve procedure helps you lose weight
in a few ways, so you have the restriction.
So this new, smaller stomach significantly
reduces the amount of food and calories that can be consumed in a sitting.
You're also going to feel full sooner with a smaller amount of food.
There are also hormonal changes, so it also causes favorable changes
in your gut hormones, which help kind of minimize your appetite,
again, improve that feeling of satiety soon after eating, and also has been shown
to have significant improvements on your blood sugar management.
With this, we don't really have as much malabsorption, but we still need to take
supplements because certain vitamins and minerals are
still impacted in how they're digested and absorbed.
And we're also eating less food.
Then we have the root on why gastric bypass.
Again, another laparoscopic surgery,
which involves often six small incisions in your abdomen.
So, with this, your stomach is made into a small pouch about the size.
Of an egg, and then your small.
Intestine is attached to it.
So here we're going to bypass the duodenum
and the jujinum is attached to your new stomach pouch.
So you're bypassing the duodenum, but your.
Stomach still remains in your body, and.
The remnant of the stomach still produces
important enzymes for digestion, which travel through the duodenum and
which is connected to the pancreas, which kind of delivers
your enzymes and bile lower down where that y connection is.
So I don't know if I can try and get
my pointer, if you can see it on whatever screen you are.
Let's see if I can get my pointer.
Oh, there we go.
So I'm going to go to pointer. Let's see.
Laser pointer.
So here the duginum is connected
to the stomach and then the duodenome is connected back to the intestine.
So this is what we would call the common
channel, where we're bypassing a certain amount
and we're having the food and enzymes kind of digest later.
So kind of, there are signals
all along your digestive tract where it's like, no, you're still digesting food.
There's food in here.
So helping you feel full longer.
Also, because you have this small pouch,
we have the restriction factor and we also have an impact on appetite hormones.
So the rudoligastric bypass is actually considered the gold standard for bariatric
surgery, as it has significant weight loss.
All right, then we have
the biliopancreatic diversion and duodenal switch.
So here it's done in kind of, it's a more complex procedure.
And this is actually saved for people
who have often a body mass index of about higher than 50.
So these are people living in really large bodies.
And so with these procedures, we have even more malabsorption and it induces weight.
Loss, even more weight loss.
So here we start by doing a sleeve gastrectomy.
As you can see from the photo,
again, kind of 75, 80% of the fungus of the stomach is removed.
So here this approach results
in a restriction and a reduction of absorption of food.
So after the stomach.
So this is often done in two surgeries.
So they'll do a sleeve gastrectomy
and then they'll do the second part of the surgery.
The name the duodenal switch comes
from the fact that in this operation, the intestinal bypass starts at the duodenum.
So here we've got the duodenum.
So now we have that sphincter.
So a lower part of the intestine.
Is attached to the stomach, and then.
Another part, that part where it was removed, is attached lower down.
So we have even a smaller common channel,
so even more malabsorption of the food and a smaller area of digestion.
So here we have the restriction, and we have an impact on appetite
hormones, and we also have reduced absorption of micron
macronutrients, contributing to more weight loss.
So here there's actually two.
So here they've got to reattach at the sphincter and the intestine,
and then they need to do a reattachment here at this bottom part.
And the reason why I'm mentioning that is that the new surgery on the block
that was approved by the American Society of Metabolic and Bariatric Surgery
is called the single anesthemosis duodenal ilio bypass with a sleeve gastrectomy.
So it's called a Saddi.
So with the Saddi, again,
kind of the new surgery on the block, supposedly it has less complications than
the biliopancreatic diversion and duodenal switch.
So this is kind of a modified version of the previous surgery.
So again, here we do the sleeve
gastrectomy, where 70% to 80% of the fungus
of the stomach is removed, and then the duodenum.
The duodenum is
cut, and then we have a lower part of the intestine that is attached.
So there really is just one cut and attachment here.
So pretty much a lower part of your
intestine is now attached, kind of, to the gastric emptying of your stomach.
I hope I'm explaining that.
Okay, so here you're getting your enzymes
that are still coming in, but they're not getting mixed till later on.
So this is your common channel here,
which is just going to be the lower part of the intestine.
So again, we have the restriction.
So you're going to feel having less food,
and then we're going to have a certain amount of malabsorption.
So again, here we're only having kind
of one cut and attachment, where the previous surgery, we had two.
Okay, so, bit more information from Richmond.
So the gastric bypass is, aGain, kind of the preferred bariatric surgery
that they perform and is still kind of the gold standard.
They want patients, again, to keep an open mind to the different
surgical options so the surgeons can discuss the best option for you.
Now, we have patients often asking, what surgery should I get?
Well, it really depends on kind of your age, your weight, how much weight you want
to lose, and what other medical conditions you have.
So it's really hard for us to say this is
the surgery, but you definitely need to be familiar with the different surgeries.
And patients who are interested
in the SADI or the BPD follow a bit of a different pathway,
as they would need to be screened and optimized by their endocrinologist, Dr.
Capad Ludo.
And they are very selective with patients pursuing this route.
Again, you need to have a higher body mass index of 50 or above.
So people with higher weights and larger
bodies, they're going to have, and they need more significant weight loss.
So there's a more of a significant impact on their health and medical conditions.
And again, you need to be quite motivated for these surgeries.
Only Dr.
Sampath at the Richmond program does the SADDI or the BPD.
So there's actually a longer wait for these surgeries.
And people wanting to undergo the SADI or the BPD.
Again, just a couple of notes, need to be very compliant.
There's more absorption,
so complications and nutritional deficiencies are definitely possible.
People, again,
need to be kind of compliant with their appointments, nutrition, eating behaviors,
taking medications and supplements every day.
And there's also these surgeries
from last I heard, the BPT actually with having to consume
extra supplements, extra protein, dealing with some of the bowel issues.
It's about $150 cost.
So they will assess that with you?
Yeah, per month.
So that's something to keep in mind.
Again,
they're very selective on who pursues the surgery, and it's something that they
would talk to you about once you get there.
So again, we work with the RichmonD metabolic and bariatric surgery program.
That said, we've had a couple patients go
through the Vancouver island program with Dr.
Amson and Dr. Malik.
We also have patients that are looking
for revisional surgery because they've had another.
Bariatric surgery and they've experienced weight regain.
Or they're looking at a revision or they're having issues.
So our role is to assess readiness
for surgery, prepare patients, and support them post bariatric surgery.
So we provide long term bariatric care.
We see our patients every six months, the Richmond Metabolic bariatric surgery.
Once you get to them, their team.
Also needs to assess your appropriateness for surgery.
And if it's safe, they're going to do the surgery.
And they kind of provide immediate and post surgical care.
And they're the ones, they have the surgeons who actually do the procedure.
So kind of looking at the bariatric program.
Right.
Everyone needs to do core, which we now call our trailblazing.
Everyone here would have done the medical
and Surgical Intervention group to learn about bariatric surgery.
And we are at the four week module.
After the four week module in time.
If you are serious about surgery
and pursuing, we have the eight week bariatric preparedness course,
which then will result, hopefully after the eight weeks, though,
doesn't guarantee nutrition and lifestyle clearance because you need to apply
the behaviors we're going to be talking about today.
After that, we have a medical review to make sure everything is stable,
which then results in your referral to Richmond.
Once you get to Richmond, probably will receive surgery in four to six months.
Again, hopefully they won't uncover.
We've had even patients,
through all their assessments find a diagnosis of cancer,
which a patient needed treatment for, or even some heart condition.
But that's if everything goes according to plan.
So you also have to meet.
So I actually have a detailed handout.
So after the email today, after the session today,
you will get all our resources about the bariatric surgery stream
and it will give you all the details of the appointments to Richmond.
So please review it because I get a lot of questions and you will be given
a resource of all our appointments and all their appointments.
Again, this is not a quick process.
Pre surgery phase takes like,
this is a surgery that you can take time to prepare for.
And so I've never have had a patient
complain to me after the process that they wish they got it right away or yesterday.
Even patients who've had the surgery
before said they wish they were better prepared or had the information.
So again, we are doing this process for your own
safety and so that you have positive long term outcomes.
You also need to complete a mental health requirement for Richmond.
So the mindfulness course is now accepted by Richmond or living Life to the full.
Also, if you do have a therapist or a psychologist, we will need a.
Letter from them in time just to.
Demonstrate your mental health stability, that it's being monitored and followed.
And then perhaps if there are any things,
if you are not cleared, then we perhaps need to figure out how we
can further support you to meet the requirements.
So, timeline, because people were asking about a timeline in the chat box.
So really it takes
one year or longer, and we've had patients in our program who've been with us four
years and then decide to undergo bariatric surgery.
So really it's up to you.
But if you've been in our program
and you're doing all the groups, probably getting through everything
about a year, I would say so again, we're assessing your readiness for change.
You need to complete all the course
requirements, kind of providing the teaching and support
to develop the skills to do well post bariatric surgery.
And we also want to make sure that you're comfortable and really prepared.
Sometimes it's just not a right time in our life, especially,
we've had many reasons for patients kind of putting things on hold.
And then post surgery, we're here to support you in your recovery
and help assist you in supporting you in maintaining your new lifestyle long term.
So I'm not going to go over this in detail
because I am going to give you this in a handout.
But just to know, when you get to Richmond,
everything is often done virtually now or over the phone for people thinking.
And if you are traveling in, they do try and put your appointments
together so you're not coming multiple times.
They're very mindful of that.
So there's the program orientation, which is in a group setting.
And then you may, that same day,
depending on how things go, be booked for a medical review with their
registered nurse, again, virtually by phone.
You have also to see their dietitian for their assessment on their part.
So even if I provide you clearance,
my goal is that you only meet with their dietitian once that you're meeting.
The requirements you're going to, if deemed.
Necessary by the surgeon, gastrointestinal scope.
You need to do kind of hospital pre
admissions where they're assessing things which would involve going to the hospital.
And then they also have pre op weigh
in and post bariatric nutrition appointments.
So again, this is done virtually.
You also need to follow a pre op diet two
to three weeks to kind of shrink your liver, which we'll talk about next week.
And then surgery people were asking,
you're about one to two days in the hospital.
Recovery is, on average for most people, return to work within four to six weeks.
And this is all from Richmond.
And then you have a post bariatric appointment one week after your surgery.
Then you have an appointment three weeks after your surgery.
Then you have an appointment six weeks after your surgery.
And then after that, they will see.
You at three months. Six months.
And then if everything's good, you're discharged back to us for a one
year follow up or they may continue to follow with you.
So again, I have this detailed in a handout, so please review it because
I get asked all the time about appointments at Richmond.
So thinking about program costs.
So again, after surgery, you're going to have to take vitamin
and mineral supplements every day for the rest of your life.
That will not change.
So that costs about thirty five dollars
to seventy five dollars per month, depending if you're buying over
the counter or bariatric specific ones, again with the BPD or the SADI surgeries,
there's a cost that Richmond has assessed about $150 a month.
There's the Bariatric preparedness course,
which covers three food Journal reviews and other assignments.
And I run the course, and so I'm not covered under your medical service plan.
So there is a cost.
If you see Carla, our dietitian, it's $150 for an hour.
So that course is at least 2 hours of work with three food journal reviews
and the assignments and making myself available to patients.
The Richmond Manual,
I don't know if it's just available through PDF, but there was a cost
for it for $10, which you'll get when you get to the Richmond program.
And then you need to think about time off. Right.
So pre surgery classes, so you guys being right here right now,
that time and commitment, there are appointments in both our programs.
They do recommend taking about four weeks off work for post surgery recovery.
And then also post surgery,
we offer monthly bariatric support groups and other groups.
And then there was transportation costs, which I feel like now is reduced due
to COVID because a lot more things are done virtually or over the phone.
Okay, I'm going to talk about weight loss expectations in regards to surgery.
And then I think we have another question period.
So things to keep in mind are what are you looking from the surgery?
Right.
Obviously in the States, they also call it weight loss surgery,
which is now becoming known more as metabolic and bariatric surgery.
We've had patients lose like 80 to 100 pounds prior to surgery.
So really the surgery is seen more as
a weight loss maintenance tool than further weight loss.
Are you wanting to improve your medical condition?
So we know with type two diabetes it can go into remissIon?
Some people get off their sleep.
CPAP machines.
Are we wanting to prevent perhaps the development of certain chronic diseases?
Are we just looking for an improved quality of life?
So in regards to surgery, when we look at the literature,
when you're going to start to look at things online,
what you'll see are quite high percentages.
And I'm going to talk about excess body
weight loss because those numbers look really high.
And this is not total weight loss.
And I'm going to explain the difference
because it's really important when we're managing our patients expectations,
what the difference is, because the numbers look so different
from one column to the other, and you probably would agree with me.
So I'm going to explain how we calculate
excess body weight loss and then what total weight loss is.
And again, weight loss kind of continues after surgery for about most of it will
happen within your first year to about 18 months.
And then after that, we're working on maintaining that weight loss.
It's not like you're going to lose weight
forever and become a skeleton or someone very slim.
The weight loss does stop at about one
and a half years, and then your body will kind of develop this new set point.
So when we look at what excess body weight
loss is, let's take someone who is 25 years old, and they.
Weigh 350 pounds, and their height is.
About 57 or 172 cm.
So that makes their body mass index
about 53.7. Just trying to get.
Next.
All right, so then what would their body weight?
And our goal with bariatric surgery is not to get to a body BMI of 24.9,
but that's kind of what they use when they're looking at kind.
Of excess body weight.
So they look at for that person who's age
25 and is 57, with a BMI of 24.9, what would their weight be?
So their weight would be 163 pounds.
So what we then do is we take their weight at the BMI of 53.7, which is 350 pounds,
and we minus their weight at a BMI of 24.9, which is 162.
And so that difference is 182 pounds.
So that's what, in the bariatric surgery
world, we kind of consider as excess body weight.
So they take that 182 pounds, and they multiply that by zero point 65,
which would be that kind of 65% on the previous slide.
And so it's possible that somebody would lose 118 pounds.
Right? So that would be that 65% of excess body
weight loss would be possibly a weight loss of 118 pounds.
We do not see 100%, like people have asked
me before, do we see 100% of excess body weight loss?
I have honestly seen that, like, one case, it's not the average.
And we'll talk about long term weight. Loss in week three,
kind of talk a bit more about managing expectations and numbers.
But 118 pounds could be lost,
350 minus that, 118 pounds you could lose from surgery.
Your weight loss could be and may.
Come to 232 pounds achieved post surgery,
because we know that weight loss goes up to 18 months.
So your BMI will still be 36.3.
Which still puts it, again,
we don't often use BMI because it really doesn't tell us anything.
About your health, because at that BMI, you're going to be a lot healthier than
at your BMI of 53.7. You're probably going to be able to feel better and move your
body in better ways than being at a weight of 232 versus 350.
So when we look at actual or total weight
loss, which would be if we did 350 minus the 232 pounds
divided by the 350, then we get total weight loss.
So your actual total weight loss would be 33%, which is a lower number than what we
would see as excess body weight loss of 65%.
So I hope that explains it a bit.
Because a lot of what you're going.
To see online, when you look at different
weight loss calculators or things, they look at excess body weight loss.
So 65% of total weight loss is not something we see.
Again, that's 65% of that excess body weight loss.
So if we kind of are looking at.
So here, just to give you an idea where your weight loss may go,
I have on the left a column of your possible presurgery weight.
So we often base this on what is
the weight that you are right before undergoing bariatric surgery.
We're not talking about your highest
weight or even the weight when we're going to refer you to Richmond.
This is all based on what we call, like, the weight right before your surgery.
So if your starting pre op weight is, let's say, 300 pounds,
if you go across the column to the green section, if you lose about 20% to 35%
of your total actual weight loss, you will be between 195 to 240.
Pounds, which is a weight loss of.
About 60 to 105 pounds.
Now, the other thing to notice on here is
the higher weight you are, the more weight you will lose.
Because we use percentages,
we don't say how much weight you're going to lose in pounds from the surgeries.
What we see is percentages.
So if you weigh 225 pounds, you are going to lose not as much weight
as someone who is 350, but that person who is 350 needs to lose
more weight than someone who is 225 pounds.
Because somebody who is 225 pounds, if they lost 100 pounds,
they would only be 125 and perhaps very unwell and anorexic, possibly.
So it is a percentage.
And so we also want to be mindful when
we're talking to other people who've had surgery or looking at social media
and people are, like, saying how much weight they've lost.
Again, we really need to look
at percentages because that comparitis can negatively impact us and make us feel
that we haven't done well from the surgery when we actually have done very well.
So something to really keep in mind,
and this is something we'll review again in the bariatric preparedness course,
because it's really important in managing our patients expectations.
All right, so this is actually another slide or handout from the Richmond Manual,
and they, again, provide this to their patients.
So here with the sleeve gastrectomy,
it says, average one and a half year weight loss is about 25%.
Gastric bypass is about 35%.
And again, with the SAddi
and the biliopancreatic divergence, you can see about 50% of total weight loss.
Right.
So for the gastric bypass,
if your starting weight is 300, your mean average post bariatric surgery
weight loss and maintenance would be about 100 pounds.
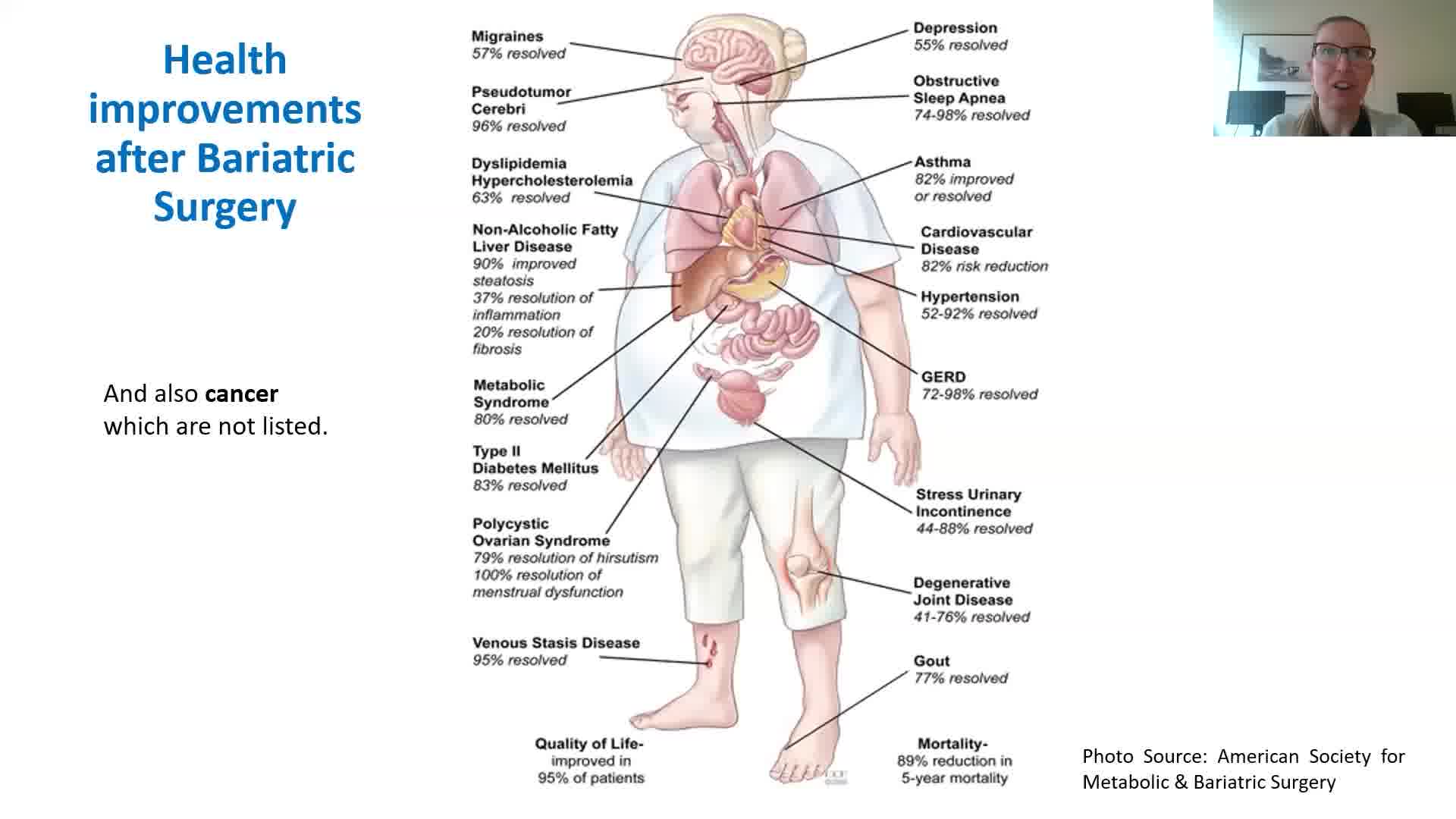
But besides that, I think what's more important is
the health improvements after bariatric surgery.
So, again, this kind of gives us an idea of things.
So there are certain,
definitely comorbidities that are associated with carrying excessive
and abdominal or dysfunctional fat on the body.
And so we see, again, I mentioned type two diabetes in remission.
We can see reductions in nonalcoholic fatty liver disease.
We can see resolve, perhaps not everyone's sleep apnea, the new kid on the black.
And more research is coming out on reduced
cancer risk, improved quality of life, reduced mortality.
So so many benefits above and beyond.
Just a change in weight, as Dr.
Galindo or they've discussed
in the medical and surgical group, age is 18 to 65.
That said, we have referred some people above 65.
It's really on an individual basis, but that's kind of the general eligibility.
We talked about a BMI of 35.
With a weight related disease or over 40 also.
So people were asking about clearance.
You have to have no significant
cardiopulmonary or medical cormobidity that requires additional assessment.
So kind of all your health conditions need to be managed and stable.
Again, no history of significant gastrointestinal diseases.
If you do have a significant gastrointestinal disease
and followed by a gastroenterologist, Richmond will require a letter saying
that it's okay for you to pursue bariatric surgery, no previous gastric surgeries.
That said, obviously, if you've had bariatric surgery and you're
looking at a conversion or revisional surgery, that is an option
not using or dependent on non steroidal antiinflammatories.
So we need to transition patients off these medications.
NSAIDs, as they're called, can increase the risk of ulcers.
So we need medications like Tylenol.
Again, if you're using it really
occasionally and you need to use NSAIDs, it may be okay.
But again, if you live with chronic pain,
you need to talk about a plan of different medications to use.
And then the last one is your BMI needs to be 60 or below.
If your BMI is over 60, then we need to help you and work with you.
And you'll meet with Dr. Lyon to lose weight.
And this has to do with their surgical equipment.
They can't work with people with a BMI higher than 60.
And especially if there's complications, we need to think about the machines
and what they can tolerate in regards to body size.
So we will work with you and alongside
with you to get your body mass index down to 60.
And we've done this for other patients also, so I guess that's the only time
weight loss may be required prior to bariatric surgery.
All right.
If you have type two diabetes or type one,
we need to make sure that your hemoglobin, a one C, is 8.5 or below.
So we might need you to work.
With our diabetes team if you have.
Everyone who wants surgery needs to be assessed for sleep apnea.
So Phil will review this and reach out to those people if they haven't.
And if you have sleep apnea,
you need to be compliant with your CPAP or BIPAP machine.
We will need a compliance report.
If you are a smoker, you actually need to be smoke free for six months.
The reason for that is that nicotine can
increase the risk of ulcerations, and it's also a surgical risk.
And Richmond will do random checks,
so complications are significantly increased due to smoking.
There's also the risk of a leak
from the connection that is higher because smokers may not heal properly.
And also, you're at an increased risk of deep venous thrombosis.
So you need to be smoke free for six months.
Or if you vape, you need to be vape free for six months.
So that might be something you need to start, or perhaps you have started.
Already in regards to.
I'll talk about cannabis in the next slide.
Other chronic metabolic issues also need to be well treated.
So your blood pressure, dyslipidemia, hypothyroidism.
All right, so cannabis.
So smoking or vaping cannabis must be stopped six months before referral.
However, edibles and tinctures as
alternatives for medical use or medical cannabis are okay.
And then that will be further discussed when you get to Richmond.
So, again, edibles and tinctures as
medical cannabis are all right, but no smoking or vaping.
So I hope that clears that up.
And then mental health.
So again, we want to make sure that there's no
history of self harm or suicide, as this can increase.
Post bariatric surgery.
There's kind of two major things
after surgery we want to manage is suicide, and the other one is
the possibility of the development of an alcohol use disorder.
If you do have a mental illness, we need
a substantial period of mental health stability of at least two years documented
by your mental health professional or GP treating the mental illness.
And a letter will be asked,
you need to stop using any non prescription or illicit drugs.
One and a half years, 18 months before surgery.
And I believe they do checks also.
So that's something to be very mindful of.
No cognitive or personality disorder or
substance abuse disorder that could affect compliance with treatment.
So some of patients may be with bipolar or other mental health illnesses.
Again, this is kind of on an individual
basis, and those patients will be assessed by Dr.
Lyon.
ADHD.
Again, how is it treated?
How are you managing?
We have patients who have had ADHD
and have had surgery, no active binge eating disorder.
So again, that it's being managed and not currently.
And again, in the eight week course,
we talk about how that may translate after bariatric surgery.
And then you need to complete one of our
cognitive behavior therapy programs, like living life to the full
or the eight week mindfulness course, and demonstrate a good compliance,
adherence with medical appointment and treatment recommendations.
All right.
And then I'm going to jump into the lifestyle and nutrition recommendations.
Sometimes I have patients asking, oh, should I start on this now?
And I say yes, because then when you get
to the bariatric preparedness course, it'll be a lot easier.
And I'm fine tuning your nutrition
and eating behaviors to meet the requirements.
So if you want to kind of self assess yourself.
And as I'm going through this, are you doing these things?
You can kind of do a bit of a check in.
Right.
So with Richmond, you need to be food journaling every day,
whether it's a pen and paper word document.
Myfitness Pal Bariastic, they want you to be food journaling every
day because research shows that those who track their dietary intake tend to be
more successful, have better success in regards to their weight loss outcomes.
Right. So it kind of takes the autopilot.
It helps us become more aware and in charge of our food and eating decisions.
Again, we come to a place of it of curiosity instead of judgment.
It allows you to determine if you're eating enough protein for your needs,
which becomes really important after surgery.
It can help you see patterns
and identifying kind of challenging times to help you develop solutions.
So tracking becomes really important.
If you hate food journaling,
something that you can reach out to me during the bariatric prep course,
and we can talk about different ways, but this is really important.
The other is kind of balanced plate.
So eating balanced meals, so protein with every meal and snack.
Vegetables at least twice a day, fruit once a day is really important.
And not eating out more than twice a week.
Richmond wants you eating more mindfully, slowly chewing food.
Well, it should take about 20 to 30 minutes to eat your meal.
So when I'm clearing patients, they need to be towards 20 minutes
of eating their meals, their main meals of breakfast, lunch and dinner.
And then you also need to develop kind of a structured eating time.
So breakfast within 60 to 90 minutes
of waking up, and then meals and snacks within two to four hour range.
Remember, after surgery, you're limited in how much food you can have in a sitting.
So you kind of need to eat four to six times during the day.
And yes, you need to work on trying this out and doing this now.
Richmond wants patients to have these
behaviors in place so that you know you'll be able to eat this way after surgery,
but also to kind of set new rhythm in routines and that foundation.
So as you're recovering from surgery
and dealing with other things, you have this good base.
So you need to be starting to work.
So for clearance, you need to be eating this way.
You need to work towards consuming one
and a half to two liters of calorie fluids per day.
So that's water, decaf tea or decaf coffee in time.
During the bariatric prep course, you need to eliminate sugar sweetened beverages.
No carbonated beverages.
No alcohol or caffeinated beverages after surgery.
Caffeine can exacerbate heartburn, so they want people off caffeine.
Carbonated beverages make you feel horrible and don't feel very well.
No alcohol again for the ulcer.
And you're at an increased risk of alcohol use disorder.
So it's actually recommended not to drink alcohol for the first year after surgery.
And also you need to remove any kind
of sugar sweetened beverages because of the possibility.
In time, we'll talk about dumping
syndrome, which someone mentioned in the chat box.
So these are the requirements for Richmond.
Decaffeinated tea and coffee is allowed.
You also need to work in time on separating your solids and liquids
by 30 minutes with the gastric bypass, you don't have that lower sphincter.
You're also really limited in how much food you can eat in a sitting.
So we don't want to combine fluids
and solid food together and not eating out more than twice per week.
So when we talk about a balanced plate, again, it doesn't matter if you're
following a whole food, plant based, vegan or kind of a low carb, higher fat diet.
What's most important?
When I assess patients in the bariatric preparedness course,
I just need to see a protein rich food with all your meals and snacks.
Vegetables need to be eaten at two separate meals per day.
So perhaps lunch and dinner or dinner and an afternoon snack.
Fruit needs to be consumed at least once
per day, and then we're looking for healthy fats and high fiber foods.
After surgery, you eat protein, produce, and lastly your carbohydrates.
So again, we're getting used to making
sure we're getting our protein throughout the day, getting our produce throughout
the day, and then carbs, if you eat carbs or not.
So protein becomes really critical after surgery because it really helps the body
heal, it helps with satiation, it helps with your metabolism.
So depending on your height,
we want to make sure that you're meeting your protein requirements.
So that's what this slide shows is if you're taller than 6ft, my apologies.
I will tell you what your protein requirement is,
but this is kind of the range, and I would kind of aim for the middle of the road.
So with meals and snacks,
we want about 18 to 30 grams of protein and snacks about five or 4 grams to 15.
So the idea is really to have a good
protein spread throughout the day is the key there.
And again, somebody was asking, well, what about Clarence?
So all those items are on this document,
which I will complete after the bariatric prep course,
to provide nutrition and lifestyle clearance.
Right. So you can already get a sense,
as I went over those items, whether or not you're applying them.
And if you are already, then that's great.
And maybe you need to work on.
Some things.
Then we have movement, which is really important.
So if you are obviously, there are people living with limitations,
disabilities, obviously, if you're in a wheelchair,
you need to think about how you may be able to move your body.
For some people,
it may also be their movement, maybe the house chores that they do,
because perhaps they're living with chronic fatigue.
So again, this is kind of assessed on an individual basis,
but if you are able, Richmond wants patients who are undergoing
bariatric surgery to move their body about 30 minutes every day.
That could be in ten minute intervals, and we can discuss that more in time.
But again, movement really helps maintain weight loss after surgery,
and resistance training is very important for us to maintain as much of our lean
muscle mass because obviously with weight loss, we'll lose some.
Of that and then sleep is really critical.
So again, if you haven't been assessed for sleep apnea, everyone who will undergo
surgery, we will reach out to them and order a sleep study.
And if you are on a CPAP and require it, we will need a CPAP report.
And then again, mental health.
If required,
we will ask for a letter from your counselor, psychologist or psychiatrist.
Richmond will reach out to your family doctor.
I think one thing to really be mindful of,
that problems don't go away with weight loss.
Life still happens, and just because you're a smaller size.
I've had patients in the past think about how their life is going to be
after, and they are surprised that things are still the same sometimes.
So again, something to think about.
Some patients struggle after with body
image and body dysmorphia when they see their excess skin after bariatric surgery.
So we talk a little bit more
in the bariatric preparedness course about kind of the mental health changes besides
just the weight loss changes associated with surgery.
And then if you're somebody who likes to have
things packaged and likes to read, because obviously in these presentations,
we're giving you bits and bytes, these would be some recommended books
that you could read as you prepare for bariatric surgery.
One of my favorite ones is the book in the middle.
And even though they're a bit dated,
a lot of the information is still the same, to be quite honest.
And so the one in the middle is written
by a dietitian, an MD, and also has some recipes.
All right, so next week we're going
to chat about kind of getting to the point of being cleared for surgery and what kind
of the immediate post surgery phases look like till six months.
I will briefly talk about skin removal surgery in week three.
See you all next week.
And, yeah, have a good week.
Bariatric Surgery Medical and Lifestyle Requirements
Getting Serious About Surgery
1. Bariatric Surgery Explained
2. Different Surgeries
3. Bariatric Preparedness
4. Sleeve Gastrectomy
5. Balanced Foods
00:00:00
00:09:09
00:19:47
00:29:31
00:39:42
We’ll explore key aspects of bariatric (weight-loss) surgery, focusing on understanding the surgical options, dietary and lifestyle requirements, and the support systems needed for successful outcomes. Bariatric surgery is an option for managing obesity, especially when traditional approaches haven’t achieved sufficient weight loss or improvements in related health issues.
This module begins by examining four types of bariatric surgery offered by the Richmond Metabolic and Bariatric Surgery Program. These include the sleeve gastrectomy, Roux-en-Y gastric bypass, biliopancreatic diversion with duodenal switch, and the newer single anastomosis duodeno-ileal (SADI) bypass. Each procedure varies in how it impacts the stomach and digestive system, influencing food intake, nutrient absorption, and appetite control through hormonal changes.
We’ll discuss pre-surgery criteria, including body mass index (BMI) guidelines, health assessments, and mental health stability. Candidates for surgery must demonstrate readiness through lifestyle changes, such as mindful eating, food journaling, structured eating times, and meeting specific physical activity and fluid intake goals. Additionally, there are dietary requirements and specific restrictions on smoking, alcohol, and certain medications to reduce surgical risks and support post-surgical health.
By completing this module, you’ll gain a foundational understanding of bariatric surgery and be better prepared to decide if this path aligns with your health goals.
Resources
Session 1: Bariatric Surgery Medical and Lifestyle Requirements Slides
Post session Handouts
Bariatric Surgery Resources
MMWMC Bariatric Surgery Resource Documents
Richmond Appointment Handout
Richmond Metabolic and Bariatric Surgery Program appointment support, reference, and requirements.
Bariatric Education Feedback Form
Bariatric Education Comments and Feedback
In week one of the bariatric education module, participants receive a comprehensive overview of bariatric surgery options, eligibility requirements, pre- and post-surgery preparation, and lifestyle changes. Four types of bariatric surgeries are covered: sleeve gastrectomy, Roux-en-Y gastric bypass, biliopancreatic diversion with duodenal switch, and a newer option called single anastomosis duodenal-ileal bypass with sleeve gastrectomy (SADI). Each surgery involves reducing the stomach’s size, which limits food intake and alters digestion to promote weight loss. Specific options vary in terms of restriction, nutrient absorption, and impacts on appetite regulation.
The program emphasizes that bariatric surgery is a tool for achieving and maintaining weight loss, not a quick fix. Participants are encouraged to adopt new eating and lifestyle habits in advance. For example, they need to journal their food intake, follow structured meal timings, and consume balanced meals with adequate protein and vegetables. Physical activity and sleep hygiene are also highlighted to aid long-term success. Patients will need to avoid caffeine, carbonated beverages, and alcohol post-surgery and must separate liquids and solids by 30 minutes.
Mental and physical health stability is required for eligibility, as surgery involves significant changes to digestion and nutrient absorption. Smoking and cannabis use (smoking or vaping) must be stopped six months prior, and stable management of conditions like diabetes is essential. Mental health screening, including support letters from counselors, is mandatory to ensure readiness for the psychological adjustments post-surgery.
Patients typically undergo an extensive preparation phase, including an eight-week bariatric preparedness course, and a full medical review before referral to surgery. The Richmond Metabolic and Bariatric Surgery program provides support through virtual appointments to minimize travel. After surgery, the program assists with recovery, requiring lifelong vitamin and mineral supplements and regular follow-ups to monitor health.
Completion of this particular is not required to advance to other lessons in this module.
Please note that understanding the core concepts contained in this lesson will help ensure your success going forward. By way of review, these concepts are:
- Different types of bariatric surgeries are discussed, including sleeve gastrectomy, gastric bypass, and biliopancreatic diversion and duodenal switch.
- The importance of considering factors such as age, weight, and medical conditions when choosing a surgical option is emphasized.
- The Richmond bariatric surgery program offers virtual and phone appointments and has a lengthy preparation process before surgery.
- The transcript discusses BMI, weight loss expectations, eligibility criteria, and lifestyle and nutrition recommendations for bariatric surgery.
There are no reviews yet. Be the first one to write one.
 LESSON SUMMARY
LESSON SUMMARY Audio Only
Audio Only Completion Requirements
Completion Requirements